Difference between revisions of "Pulmonary alveolar proteinosis"
Jump to navigation
Jump to search

(+SO cytol) |
|||
| Line 125: | Line 125: | ||
</pre> | </pre> | ||
===Micro=== | ====Micro==== | ||
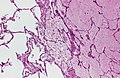
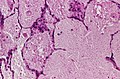
Sections show lung with eosinophilic material in the airspaces. Focally, small (~20 micrometres), more dense appearing, bodies are also in the airspace. The alveolar walls are within normal limits. No significant inflammation is identified. No microorganisms are seen with routine stains. There is no pulmonary hemorrhage. | Sections show lung with eosinophilic material in the airspaces. Focally, small (~20 micrometres), more dense appearing, bodies are also in the airspace. The alveolar walls are within normal limits. No significant inflammation is identified. No microorganisms are seen with routine stains. There is no pulmonary hemorrhage. | ||
===Cytology=== | |||
In conjunction with history and imaging, PAP be diagnosed on cytology.<ref name=pmid29607238>{{cite journal |authors=Li M, Alowami S, Schell M, Davis C, Naqvi A |title=Pulmonary Alveolar Proteinosis in Setting of Inhaled Toxin Exposure and Chronic Substance Abuse |journal=Case Rep Pulmonol |volume=2018 |issue= |pages=5202173 |date=2018 |pmid=29607238 |pmc=5828087 |doi=10.1155/2018/5202173 |url=}}</ref> | |||
<pre> | |||
Right Lung, BAL: Negative for Malignancy. Macrophages and amorphous material present in a dirty background, see comment. | |||
Comment: | |||
Satisfactory for evaluation. | |||
PAS positive and PSAD positive staining globules are present. GMS stain for pneumocystis is negative. | |||
In the proper clinical context, the findings may be in keeping with pulmonary alveolar proteinosis. | |||
In the context of possible PAP, GM-CSF testing is suggested, if not already done. Please correlate with clinical and radiologic findings. | |||
The case was partially reviewed internally. | |||
</pre> | |||
==See also== | ==See also== | ||
Revision as of 15:54, 17 April 2025
| Pulmonary alveolar proteinosis | |
|---|---|
| Diagnosis in short | |
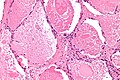
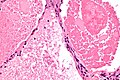
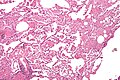
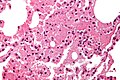
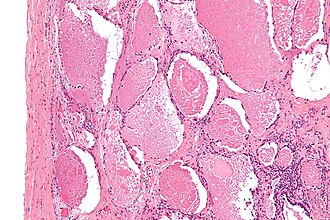 Pulmonary alveolar proteinosis. H&E stain. | |
|
| |
| LM | "dense bodies" or "chatter" (represent dead macrophages) within acellular eosinophilic material that is in the alveoli |
| LM DDx | pulmonary edema, pneumocystis pneumonia, pulmonary hemorrhage (acute), mycobacterial infection, Nocardia infection |
| Stains | PAS +ve, PASD +ve |
| IHC | surfactant +ve |
| EM | lamellar bodies |
| Site | lung - see medical lung diseases |
|
| |
| Associated Dx | +/-hematologic malignancy |
| Clinical history | +/-infection, +/-smoking |
| Signs | decreased oxygen saturation |
| Prevalence | uncommon |
| Blood work | anti-GM-CSF antibodies, LDH elevated |
| Radiology | airspace disease, "crazy paving" |
| Prognosis | benign |
Pulmonary alveolar proteinosis, abbreviated PAP, in an uncommon medical lung disease.
General
- Associated with smoking - particularily in men.[1]
Pathophysiology:
- GM-CSF (granulocyte-macrophage colony stimulating factor) signaling in macrophages/lack of GM-CSF.
- GM-CSF is required by alveolar macrophages to clear surfactant.
Classification:[1]
- Congenital:
- Abnormal surfactant.
- GM-CSF receptor defect.
- Secondary:
- Infections.
- Haematologic malignancy.
- Acquired:
- Dusts - interfere with macrophage function.
Clinical:
- Dyspnea & cough - gradual onset.
- Anti-GM-CSF antibodies - usually.[2]
- Serum LDH elevated.[2][3]
- Decreased oxygen saturation.
Gross

Chest CT showing crazy paving pattern. (WC/Verma)
- Consolidation.
Radiology
- CXR: airspace disease.
- HRCT: "crazy paving".
Microscopic
Features:
- Crap in the alveoli:
- "Dense bodies" - dead macrophages ("Chatter" in the alveoli).
- Edema - has pink stuff in the alveoli like PAP but no dense bodies.
DDx - may mimic:[4]
- Pulmonary edema.
- Pneumocystis pneumonia - exudates foamy & vacuolated.
- Pulmonary hemorrhage (acute). (???)
- Mycobacterial infection.
- Nocardia infection.
Images
www:
Images of DDx (pulmonary edema):
Stains
- PAS +ve -- material in airspace (surfactant).[6][7]
- PASD +ve[8] (red[9]).
- Pulmonary edema fluid -ve.[10]
- Occasionally, PAP may be PASD -ve.[11]
IHC
- Surfactant +ve.[12]
EM
- Lamellar bodies.[13]
Note:
- Lamellar bodies are also seen in secreting adenocarcinoma, obstructive pneumonitis.
Sign out
LUNG, RIGHT UPPER LOBE (ABNORMAL AREA ON CT), WEDGE RESECTION: - PULMONARY ALVEOLAR PROTEINOSIS, SEE COMMENT. - NO SIGNIFICANT INTERSTITIAL FIBROSIS. - NO SIGNIFICANT INFLAMMATION. - NEGATIVE FOR MALIGNANCY.
Micro
Sections show lung with eosinophilic material in the airspaces. Focally, small (~20 micrometres), more dense appearing, bodies are also in the airspace. The alveolar walls are within normal limits. No significant inflammation is identified. No microorganisms are seen with routine stains. There is no pulmonary hemorrhage.
Cytology
In conjunction with history and imaging, PAP be diagnosed on cytology.[14]
Right Lung, BAL: Negative for Malignancy. Macrophages and amorphous material present in a dirty background, see comment. Comment: Satisfactory for evaluation. PAS positive and PSAD positive staining globules are present. GMS stain for pneumocystis is negative. In the proper clinical context, the findings may be in keeping with pulmonary alveolar proteinosis. In the context of possible PAP, GM-CSF testing is suggested, if not already done. Please correlate with clinical and radiologic findings. The case was partially reviewed internally.
See also
References
- ↑ 1.0 1.1 Trapnell BC, Whitsett JA, Nakata K (December 2003). "Pulmonary alveolar proteinosis". N. Engl. J. Med. 349 (26): 2527-39. doi:10.1056/NEJMra023226. PMID 14695413. http://content.nejm.org/cgi/content/extract/349/26/2527.
- ↑ 2.0 2.1 Lin, FC.; Chang, GD.; Chern, MS.; Chen, YC.; Chang, SC. (Jun 2006). "Clinical significance of anti-GM-CSF antibodies in idiopathic pulmonary alveolar proteinosis.". Thorax 61 (6): 528-34. doi:10.1136/thx.2005.054171. PMID 16517574.
- ↑ Bhattacharyya, D.; Barthwal, MS.; Katoch, CD.; Rohatgi, MG.; Hasnain, S.; Rai, SP.; Arora, A. (Jan 2013). "Primary alveolar proteinosis - A report of two cases.". Med J Armed Forces India 69 (1): 90-3. doi:10.1016/j.mjafi.2012.02.016. PMID 24532945.
- ↑ Leslie, Kevin O.; Wick, Mark R. (2004). Practical Pulmonary Pathology: A Diagnostic Approach (1st ed.). Churchill Livingstone. pp. 248. ISBN 978-0443066313.
- ↑ Leslie KO (May 2009). "My approach to interstitial lung disease using clinical, radiological and histopathological patterns". J. Clin. Pathol. 62 (5): 387–401. doi:10.1136/jcp.2008.059782. PMC 2668105. PMID 19398592. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2668105/.
- ↑ Ben-Dov, I.; Segel, MJ. (Jan 2014). "Autoimmune pulmonary alveolar proteinosis: Clinical course and diagnostic criteria.". Autoimmun Rev. doi:10.1016/j.autrev.2014.01.046. PMID 24424195.
- ↑ Mikami, T.; Yamamoto, Y.; Yokoyama, M.; Okayasu, I. (Dec 1997). "Pulmonary alveolar proteinosis: diagnosis using routinely processed smears of bronchoalveolar lavage fluid.". J Clin Pathol 50 (12): 981-4. PMID 9516877.
- ↑ Maygarden, SJ.; Iacocca, MV.; Funkhouser, WK.; Novotny, DB. (Jun 2001). "Pulmonary alveolar proteinosis: a spectrum of cytologic, histochemical, and ultrastructural findings in bronchoalveolar lavage fluid.". Diagn Cytopathol 24 (6): 389-95. PMID 11391819.
- ↑ Meng, ZL.; Liu, HR.; Liang, ZY.; Zhang, SY. (Sep 2005). "[Pathologic feature and diagnosis of pulmonary alveolar proteinosis].". Zhonghua Bing Li Xue Za Zhi 34 (9): 575-8. PMID 16468308.
- ↑ URL: http://pathhsw5m54.ucsf.edu/overview/fungi1a.html. Accessed on: 3 March 2014.
- ↑ Hwang DM. April 1, 2014.
- ↑ Albores, J.; Seki, A.; Fishbein, MC.; Abtin, F.; Lynch, JP.; Wang, T.; Weigt, SS. (Jun 2013). "A rare occurrence of pulmonary alveolar proteinosis after lung transplantation.". Semin Respir Crit Care Med 34 (3): 431-8. doi:10.1055/s-0033-1348472. PMID 23821516.
- ↑ Luo, BF.; Li, HP.; Yi, XH.; Tao, JW.; Lü, HJ.; Fang, X.; Zhang, ZM.; Zhang, L. et al. (Dec 2012). "[The ultrastructural features of sputum deposition and its value in the diagnosis of pulmonary alveolar proteinosis].". Zhonghua Jie He He Hu Xi Za Zhi 35 (12): 887-91. PMID 23328177.
- ↑ Li M, Alowami S, Schell M, Davis C, Naqvi A (2018). "Pulmonary Alveolar Proteinosis in Setting of Inhaled Toxin Exposure and Chronic Substance Abuse". Case Rep Pulmonol 2018: 5202173. doi:10.1155/2018/5202173. PMC 5828087. PMID 29607238. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5828087/.