Lymph node metastasis
Jump to navigation
Jump to search
| Lymph node metastasis | |
|---|---|
| Diagnosis in short | |
|
Template:Px Lymph node metastasis (colorectal carcinoma). H&E stain. | |
|
| |
| LM | malignant cells foreign to the lymph node - typically subcapsular sinus; morphology dependent on specific cancer |
| Subtypes | dependent on primary tumour - macrometastasis, micrometastasis, isolated tumour cells |
| LM DDx | endometriosis, ectopic decidua, endosalpingiosis, melanocytic nevus, dermatopathic lymphadenopathy, sinus histiocytosis, tumour deposit (dependent on site), pathology of the lymph node - see lymph node pathology and lymphoma |
| Stains | dependent on tumour |
| IHC | dependent on tumour |
| Gross | enlarged lymph node, esp. spherical, white mass with an irregular border +/-extension into surround adipose tissue |
| Grossing notes | yt? |
| Site | lymph node - see lymph node pathology |
|
| |
| Clinical history | +/-suspicion of cancer |
| Signs | +/-nodule at site of a lymph node |
| Prognosis | dependent on specific type of cancer, +/-number of nodes affected |
| Clin. DDx | reactive lymphadenopathy, lymphoma, other benign causes of lymphadenopathy - see lymph node pathology |
| Treatment | dependent on underlying cancer |
Lymph node metastasis is cancer that has spread to a lymph node.
General
- Determination of lymph node status is one of the most common indications for the examination of lymph nodes.
- It is a good idea to look at the tumour (if available) ...before looking at the LNs for mets.
- Lymph node metastasis, in the absence of other metastases, often up-stage a cancer from stage II to stage III.
Gross
- Outside:
- "Large" - size varies by site.
- Neck >10 mm.[1]
- Shape - round more suspicious than oval.
- "Large" - size varies by site.
- Sectioned:
- White firm lesion with irregular border - classic appearance.
- Non-fatty hilum.[1]
Microscopic
Features:
- Foreign cell population - key feature.
- Classic location: subcapsular sinuses.
- +/-Cells with cytologic features of malignancy.
- Nuclear pleomorphism (variation in size, shape and staining).
- Nuclear atypia:
- Nuclear enlargement.
- Irregular nuclear membrane.
- Irregular chromatin pattern, esp. asymmetry.
- Large or irregular nucleolus.
- Abundant mitotic figures.
- +/-Cells in architectural arrangements seen in malignancy; highly variable - dependent on tumour type and differentiation.
- +/-Gland formation.
- +/-Single cells.
- +/-Small clusters of cells.
Notes:
- Cytologic features of malignancy may not be present; some tumours, e.g. gallbladder carcinoma, do not always have overt cytologic features of malignancy.
- The diagnosis is based on the fact that they are foreign to the lymph node and architecturally consistent with a well-differentiated malignancy.
- Lymph node metastases in sarcomas are uncommon; they are seen in <3% of cases.[2]
- Fatty lymph nodes (esp. fatty hilus[1]) are less likely to harbor metastases.[3]
DDx - mimics of metastatic disease:
- Endometriosis.
- Ectopic decidua.[4]
- Endosalpingiosis.[5]
- Melanocytic nevus - intracapsular or within the trabeculae.[6]
- Dermatopathic lymphadenopathy.[citation needed]
- Sinus histiocytosis - especially for the junior resident.
- Tumour deposit (discoutinuous extramural extension) - definition dependent on primary tumour (e.g. in the head & neck they are tumour replaced lymph nodes, in the colon they are considered separate and not counted as lymph nodes).
Images
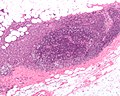
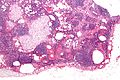
Thyroid carcinoma LN metastasis (WC)
Colorectal carcinoma LN metastasis (WC)
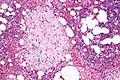
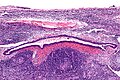
Mimics
Endosalpingiosis in a LN - very high mag. (WC)
See also
References
- ↑ 1.0 1.1 1.2 Mack, MG.; Rieger, J.; Baghi, M.; Bisdas, S.; Vogl, TJ. (Jun 2008). "Cervical lymph nodes.". Eur J Radiol 66 (3): 493-500. doi:10.1016/j.ejrad.2008.01.019. PMID 18337039.
- ↑ Fong, Y.; Coit, DG.; Woodruff, JM.; Brennan, MF. (Jan 1993). "Lymph node metastasis from soft tissue sarcoma in adults. Analysis of data from a prospective database of 1772 sarcoma patients.". Ann Surg 217 (1): 72-7. PMC 1242736. PMID 8424704. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1242736/.
- ↑ Korteweg, MA.; Veldhuis, WB.; Mali, WP.; Diepstraten, SC.; Luijten, PR.; van den Bosch, MA.; Eijkemans, RM.; van Diest, PJ. et al. (Feb 2012). "Investigation of lipid composition of dissected sentinel lymph nodes of breast cancer patients by 7T proton MR spectroscopy.". J Magn Reson Imaging 35 (2): 387-92. doi:10.1002/jmri.22820. PMID 21972135.
- ↑ Wu, DC.; Hirschowitz, S.; Natarajan, S. (May 2005). "Ectopic decidua of pelvic lymph nodes: a potential diagnostic pitfall.". Arch Pathol Lab Med 129 (5): e117-20. doi:10.1043/1543-2165(2005)129e117:EDOPLN2.0.CO;2. PMID 15859655.
- ↑ Corben, AD.; Nehhozina, T.; Garg, K.; Vallejo, CE.; Brogi, E. (Aug 2010). "Endosalpingiosis in axillary lymph nodes: a possible pitfall in the staging of patients with breast carcinoma.". Am J Surg Pathol 34 (8): 1211-6. doi:10.1097/PAS.0b013e3181e5e03e. PMID 20631604.
- ↑ Biddle, DA.; Evans, HL.; Kemp, BL.; El-Naggar, AK.; Harvell, JD.; White, WL.; Iskandar, SS.; Prieto, VG. (May 2003). "Intraparenchymal nevus cell aggregates in lymph nodes: a possible diagnostic pitfall with malignant melanoma and carcinoma.". Am J Surg Pathol 27 (5): 673-81. PMID 12717252.